
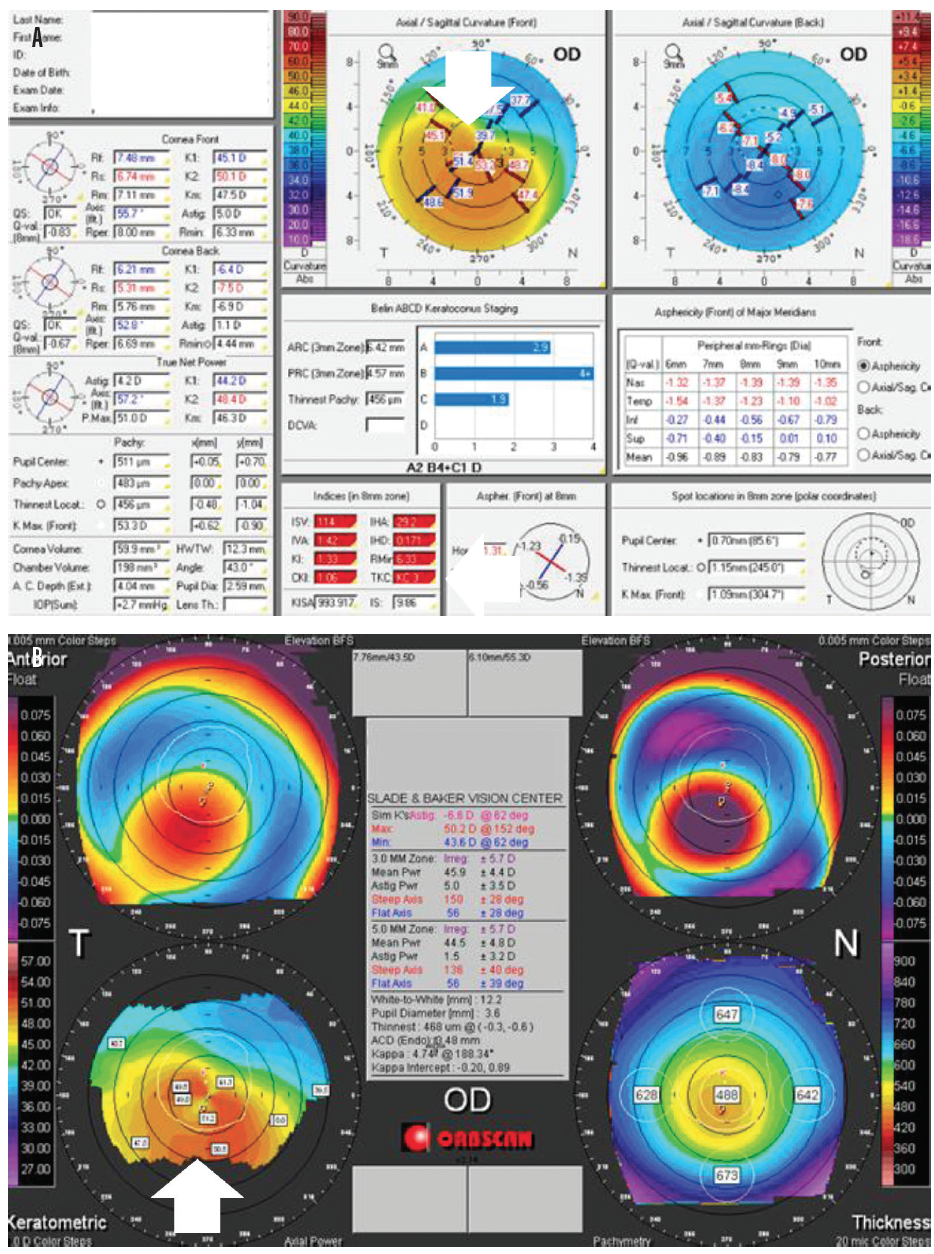
Patient was diagnosed with PMD in the right eye and scleral contact lens was advised, but patient did not use it and preferred spectacles. Left eye was completely normal with normal topography as shown in b. K1 was 37.90 D and K2 was 51.10 D as shown in a. Corneal topography (Pentacam, OCULUS Optikgerate Gmbh) showed the “crab claw sign” with against-the-rule astigmatism in OD. Fellow eye was normal on clinical examination. On examination, a crescentic arcuate reflex was seen 2 mm away from the limbus extending from 4 o' clock to 8 o'clock in the right eye. With +7.00 Diopter sphere (DS) / -12.00 Diopter Cylinder (DC) × 65°, the visual acuity improved to 6/18 in OD. Ī 64-year-old male patient presented to the clinic with painless progressive diminution of vision in the right eye since one month and was found to have a UCVA of 3/60 in the right eye (OD) and 6/6 in the left eye (OS). The corneal protrusion is more marked, just superior to the area of thinning where the thickness of the cornea is usually normal. It affects the inferior cornea mainly in a crescentic form, separated from the limbus by a relatively uninvolved area of 1 to 2 mm in width, leading to corresponding steepening and thinning which is reflected as high “against the rule” astigmatism. In a majority, it occurs bilaterally however unilateral cases have also been reported. This condition is more common in men in the fourth or fifth decades of life. Pellucid marginal degeneration (PMD) is a rare, progressive, non-inflammatory ectatic disorder of the cornea. Indian J Ophthalmol Case Rep 2022 2:882-5. An unusual case of sequential corneal perforation in pellucid marginal degeneration: A case report.

PELLUCID MARGINAL DEGNERATION HOW TO
How to cite this URL: Kodavoor SK, Patekar KB, Dandapani R. Indian J Ophthalmol Case Rep 2022 2:882-5 How to cite this article: Kodavoor SK, Patekar KB, Dandapani R. Keywords: Corneal collagen crosslinking, corneal perforation, pellucid marginal degeneration Temporal phacoemulsification with toric IOL implantation was done in both eyes, following which the left eye developed spontaneous perforation after a period of two months which was also managed with primary suturing and compression sutures.

Over a period of four years of follow-up, the patient developed progressive diminution of vision in both eyes and was diagnosed with cataract. The other eye was absolutely normal with normal topographic findings. We report a case of spontaneous corneal perforation in a 64-year-old male patient with PMD having normal corneal thickness in the right eye which was managed with primary suturing and compression sutures.
PELLUCID MARGINAL DEGNERATION SERIAL
Hence, the importance of repeated follow-up, clinical examination along with serial corneal topography even in the seventh and eighth decades of life is of utmost importance in PMD. Spontaneous and sequential corneal perforation is rare in pellucid marginal degeneration (PMD) in the seventh decade of life.


 0 kommentar(er)
0 kommentar(er)
